Wetenschappelijk onderzoek
De huidige onderzoeksprojecten focussen op het vasthouden van het effect in Nederland, het effectief inzetten van ehealth en thuismeet apparatuur, het verder in kaart brengen van de patiënten die bij ons komen revalideren en het beter begrijpen welke mechanismen aan de positieve effecten van longrevalidatie op hoogte ten grondslag liggen.
Longrevalidatie op hoogte
Het beïnvloeden van omgevingsfactoren als therapeutische optie, is door de complexiteit en matige effectiviteit van saneringsmaatregelen in Nederland enigszins uit het oog verloren. En dat terwijl juist bij de groep patiënten die ondanks maximale behandeling symptomatisch blijft dit een belangrijke rol speelt.
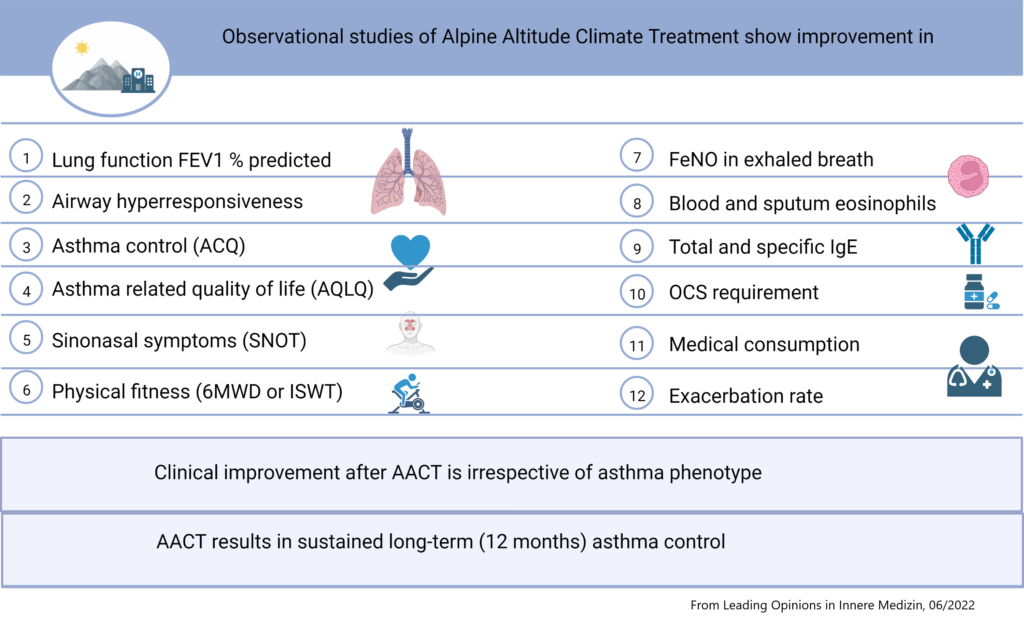
Minder huisstofmijt is niet de enige hooggebergtefactor die bijdraagt tot verbetering van de astmacontrole. Het droge bergklimaat biedt ook minder schimmelsporen, pollen en andere inhalatie allergenen. Bovendien is er minder luchtverontreiniging. De hoogte activeert verschillende immunologische processen die ervoor zorgen dat de ontsteking in de luchtwegen sneller tot rust komt. De ijle lucht zorgt voor een lagere luchtweerstand en dit vergemakkelijkt het ademen. Het zorgt ervoor dat je in het NAD effectiever kan trainen en sneller conditie opbouwt.
Longrevalidatie op hoogte biedt een unieke combinatie van omgeving, hoogte en multidisciplinaire behandeling. Doordat deze factoren gelijktijdig worden aangeboden, is het lastig ontrafelen wat de belangrijkste factor is. Wel is overtuigend aangetoond dat longrevalidatie op hoogte in veel gevallen effectiever is dan longrevalidatie op zeeniveau.
Longrevalidatie en biologicals
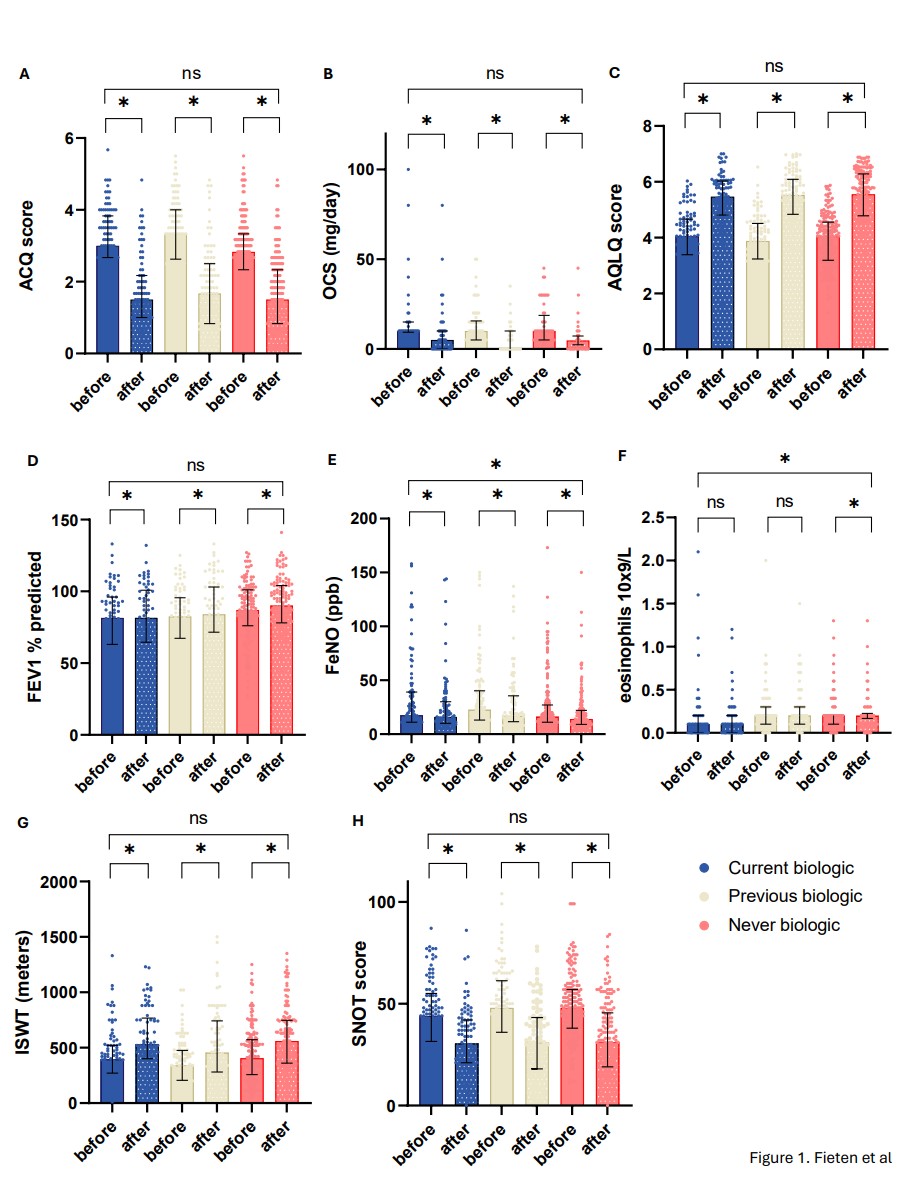
De recente ontwikkelingen op het gebied van biologicals zijn veelbelovend. Echter de huidige biologicals hebben niet bij alle patiënten voldoende effect. Dit zien we terug doordat er steeds meer patienten naar ons worden verwezen met een ongecontroleerd astma onder biological gebruik. Ook zijn er patiënten die verschillende biologicals hebben geprobeerd, maar hier onvoldoende op reageren of last hebben van bijwerkingen. Daarnaast zijn er patiënten met een ernstig ongecontroleerd astma die niet voor een behandeling met biologicals in aanmerking komen. Gelukkig kunnen we deze patiënten een revalidatie op hoogte aanbieden. Onze laatste data analyses laten zien dat de verbetering in astma controle en astma gerelateerde kwaliteit van leven vergelijkbaar is voor alle patiënten met een ongecontroleerd ernstig astma, onafhankelijk van biological gebruik. Dit is goed nieuws!
Zie ook: https://onlinelibrary.wiley.com/doi/10.1111/all.16233
Davos@home
Deze gerandomiseerde trial ondersteunt patiënten bij hun zelfmanagement in Nederland door middel van de mhealth app PatientCoach en onderzoekt de toegevoegde waarde van de inzet van thuismeetapparatuur.
In het Nederlands Astmacentrum Davos worden mensen met astma uitgebreid behandeld. Na afloop van de behandeling in Davos gaat het (meestal) erg goed met het astma. Helaas gebeurt het nogal eens dat dit bij terugkomst in Nederland niet zo blijft. Meestal gaat het langzaam steeds iets slechter. Soms komt het helaas ook voor dat mensen snel weer meer klachten hebben. Daarom willen we in de studie Davos@home een app voor uw smartphone introduceren en onderzoeken of het helpt dat mensen in Nederland thuis metingen doen. We geven een groep studiedeelnemers een longfunctiemeter (spirometer), een stappenteller (Fitbit), een FeNO meter (meet activiteit van astma in de luchtwegen) en toegang tot de app PatientCoach en een andere groep studiedeelnemers krijgt alleen toegang tot de app PatientCoach.




De app PatientCoach bevat alle informatie die in Davos is gegeven en is ontwikkeld in samenwerking met het LUMC. Studiedeelnemers maken gedurende een jaar na behandeling in Davos gebruik van de app, vullen regelmatig vragenlijsten in en doen thuismetingen. Het doel van het onderzoek is om te bepalen of het gebruik van de PatientCoach app en apparaten voor thuismetingen beter helpen het effect van de behandeling in Davos vast te houden dan de app PatientCoach zonder apparaten voor thuismetingen.
De inclusie van de trial wordt volgens de huidige planning in 2023 afgerond, de follow up duurt nog tot 2024. De resultaten van deze studie worden in 2025 verwacht. Deze studie is financieel ondersteund door de VND en de SAB.
Vermoeidheid bij astma patiënten
Veel astma patiënten die bij ons komen revalideren zijn ontzettend moe. We willen graag meer weten over vermoeidheid bij astma patiënten, omdat het een belangrijke bijdragende factor is aan een verminderde kwaliteit van leven en een vaak genegeerde uitkomst. In samenwerking met het MCL gaan we onderzoeken of een behandeling in Davos helpt vermoeidheid te verminderen en of we kunnen voorspellen bij welke patiënten dit het geval is.
NAD –
Wetenschappelijk onderzoek
NAD –
Wetenschappelijk onderzoek
NAD –
Wetenschappelijk onderzoek
Aanmelden als verwijzer
Vul als verwijzer zo nauwkeurig mogelijk het verwijsformulier in samen met de laatste relevante medische gegevens.
Ervaring van patiënt
Mijn opname in Davos heeft ervoor gezorgd dat ik de regie over mijn leven weer terug heb gekregen. Naast de schone lucht, leer je veel tijdens de workshops en biedt het programma volop mogelijkheden om zelf aan de slag te gaan met je herstel. Door dit met beide handen aan te grijpen, heb ik meer vertrouwen en hoop gekregen voor de toekomst.
Op weg naar een gezondere toekomst

Gezonde omgeving
Vermijding van patiënt relevante allergische en niet–allergische prikkels betreffen is niet een eenvoudige opgave. Met name wanneer ongecontroleerd astma samengaat met aanwijzingen van verhoogde ontsteking in de luchtwegen. Want dat is het extra van belang om factoren op te sporen die het astmatische proces prikkelen en onderhouden. Het zo goed mogelijk saneren van deze factoren blijft een belangrijke stap in astma management zowel bij patiënten met een allergisch als bij patiënten met een niet-allergisch astma. Naast de allergische en niet-allergische prikkels spelen ook de individuele gevoeligheid voor prikkels, de persoonlijke mogelijkheden om prikkels te vermijden en de perceptie van de ziekte een rol.

Zorg op maat
Een op de patiënt en het astma fenotype afgestemd behandelplan. Deze is gebaseerd op de alle domeinen van de gezondheidstoestand met persoonlijke consulten, interactieve gezondheidsvoorlichting en training sessies.
Het doel is van de behandeling in het hooggebergte is het astma onder controle krijgen. Patiënten krijgen een persoonlijk astma-actieplan mee terug naar Nederland. Hiermee kunnen ze hun chronische aandoening beter onder controle houden.
Naast de klassieke klinische behandeling van de adolescenten/jong volwassenen behandeling is kortdurende assessment en een behandeladvies mogelijk.
Assessment
Interdisciplinaire assessment van het astma fenotype, de integrale gezondheidstoestand en astma beïnvloedende factoren.